|
|
文献标题:The developmental phenotype of the great toe in fibrodysplasia ossificans progressiva.
文献作者:O. Will Towler 1,2 Frederick S. Kaplan 1,2,3 and Eileen M. Shore 1,2,4 *
1 Department of Orthopaedic Surgery, University of Pennsylvania, Philadelphia, PA, United States, | 宾夕法尼亚大学骨外科
2 The Center for Research in FOP & Related Disorders, Perelman School of Medicine, University of Pennsylvania, Pennsylvania, PA, United States, | 宾夕法尼亚大学佩雷尔曼医学院 FOP 及相关疾病研究中心
3 Department of Medicine, Perelman School of Medicine, University of Pennsylvania, Philadelphia, PA, United States, | 宾夕法尼亚大学佩雷尔曼医学院医学系
4 Department of Genetics, Perelman School of Medicine, University of Pennsylvania, Philadelphia, PA, United States | 宾夕法尼亚大学佩雷尔曼医学院遗传学系
发表时间:December 8, 2020
文献下载:点击下载
文献初译:多多爸 | 2022.08.08
多爸记:本周北京,周日深圳。本文是一篇详细讲述FOP大脚趾畸形的文章,涉及好多关于骨科的专业术语。看的实在头大,有兴趣的家长患者可以看看,估计看了也等于没看,就留给想研究骨发育的医生吧,说白了,就是论证了趾发育会受BMP信号传导的影响。就这么个事儿,发现从胎儿发育期间就开始,伴随一生,好像青春期后,有些脚趾关节还会融合。emmm,多多手指的大拇指第一节的确是融合的,但没注意观察是出生的时候就融合了,还是后期融合的,反正当时不耽误弹钢琴,早年我也没太注意她手指的问题。脚趾外翻是标准的经典型FOP的特征,两三岁的时候差点儿去和睦家做了手术,多亏当年复旦儿科的一个老大夫,问诊的时候说了一句话,我到现在还记得,他说,“这么小,手什么术,没有大脚指头都可以走路,你们瞎折腾个啥。。。”,好吧,这是多多第一次躲过介入式手术引发的FOP急性发作,好凶险。
<hr/>Abstract | 概述
进行性骨化纤维发育不良 (FOP) 是一种罕见的遗传性疾病,其中广泛的异位骨化 (HO) 会在儿童出生后开始形成,并在一生中发展。
虽然在胚胎发育过程中不会异位骨化,但是携带导致大部分FOP患者的 ACVR1 R206H 突变的儿童,在出生时会表现出大脚趾畸形,这表明该突变会影响胚胎的发育过程,进而改变骨骼的形成。
尽管大脚趾畸形在 FOP 人群中的患病率很高,但由于其临床良性的性质,这种现象所受到的关注相对较少。
在这项研究中,我们检查了 41 名年龄在 2 个月至 48 岁之间的 FOP 患者的 X 光片,以详细分析 FOP 大脚趾畸形的发育特征、进展和其变化的特点,其中包括骨骼结构的缺失、畸形的骨骺、异位骨化的核心、畸形的第一跖骨和指骨的融合。
Fibrodysplasia ossificans progressiva (FOP) is a rare genetic disorder in which extensive heterotopic ossification (HO) begins to form during early childhood and progresses throughout life. Although HO does not occur during embryonic development, children who carry the ACVR1 R206H mutation that causes most cases of FOP characteristically exhibit malformation of their great toes at birth, indicating that the mutation acts during embryonic development to alter skeletal formation. Despite the high prevalence of the great toe malformation in the FOP population, it has received relatively little attention due to its clinically benign nature. In this study, we examined radiographs from a cohort of 41 FOP patients ranging from 2 months to 48 years of age to provide a detailed analysis of the developmental features, progression, and variability of the great toe malformation of FOP, which include absent skeletal structures, malformed epiphyses, ectopic ossification centers, malformed first metatarsals and phalangeal fusion. Keywords: 关键词
关键词:进行性骨化性纤维发育不良,FOP,大脚趾畸形,拇外翻,骨骼发育,ACVR1,BMP信号
Keywords: fibrodysplasia ossificans progressiva, FOP, great toe malformation, hallux valgus, skeletal development, ACVR1, BMP signaling <hr/>INTRODUCTION | 简介
进行性骨化纤维发育不良 (FOP) 是一种极其罕见的遗传疾病,其中大量的骨组织会在软结缔组织中形成异位骨化(Shore 和 Kaplan,2010)。
导致 FOP 和异位骨化的 ACVR1 基因突变也会改变骨骼的正常发育(Cohen 等,1993;Harrison 等,2005;Schaffer 等,2005;Mishima 等,2014;Pignolo 等。 , 2019)。
FOP 患者中最常见的突变(大约97%)是 ACVR1 R206H(Shore 等人,2006;Kaplan 等人,2008)。
这个位点的突变和其他FOP有关的 ACVR1 突变增强了来自这种 骨形态发生蛋白 (BMP) I 型受体的信号传导,进而增强了下游 BMP 信号通路的激活(Kaplan 等人,2008;Shen 等人,2009;Allen 等人, 2019)。
Fibrodysplasia ossificans progressiva (FOP) is an ultra-rare genetic disorder in which extensive bone ectopically forms in soft connective tissues, such as skeletal muscle, in a process known as heterotopic ossification (HO) (Shore and Kaplan, 2010). The ACVR1 gene mutation that causes FOP and HO also alters the normal development of the skeleton (Cohen et al., 1993; Harrison et al., 2005; Schaffer et al., 2005; Mishima et al., 2014; Pignolo et al., 2019). The most frequently occurring mutation (∼97%) among FOP patients is ACVR1 R206H (Shore et al., 2006; Kaplan et al., 2008). This and other ACVR1 mutations associated with FOP enhance signaling from this bone morphogenetic protein (BMP) type I receptor to increase activation of the downstream BMP signaling pathway (Kaplan et al., 2008; Shen et al., 2009; Allen et al., 2019). FOP最为常见的先天性骨骼畸形是脚的第一趾(也称为大脚趾或拇趾),脚趾会向内倾斜(拇外翻)(Kaplan 等,2008)。
以前的报道发现,在诊断为 FOP 的患者中,第一趾的长度缩短、第一跖骨形态改变和多个轴后指(即 2-5 指)的远端指骨交联(融合)(Schroeder 和 Zasloff,1980;Harrison 等人。 , 2005);
然而,这些研究只检查了一小部分患者群体(分别为 16 名和 15 名患者)。
虽然有过对其他病例的系列报道,但却没有一个对前足畸形有足够的研究。(Rosenstirn,1918;Cohen 等,1993)。
为了调查研究所有足趾畸形的发生频率和类别,我们对 41 名具有 ACVR1 R206H 突变的 FOP 患者的 X 光片进行了详细分析。
The congenital skeletal malformation most commonly associated with FOP affects the first digit of the foot (also called the great toe or hallux), with this toe angled inward (hallux valgus) (Kaplan et al., 2008). Previous reports identified reduced first digit length, altered first metatarsal morphology, and distal phalangeal coalition (fusion) in multiple post-axial digits (i.e., digits 2–5) in patients diagnosed with FOP (Schroeder and Zasloff, 1980; Harrison et al., 2005); however, these studies examined only small cohorts (16 and 15 patients, respectively). While other case report series have been conducted, none have focused extensively on the forefoot malformations (Rosenstirn, 1918; Cohen et al., 1993). To investigate the frequency and types of malformations in all the digits of the foot, we conducted a detailed analysis of radiographs from 41 FOP patients with the ACVRIR206H mutation. MATERIALS AND METHODS | 材料和方法
。。。
RESULTS | 结果
在可用的 FOP 病例文件中,记录了41 名受试者为常见的 FOP ACVR1 R206H 突变(男性22人,女性19人;年龄 0-48 岁),临床诊断为 FOP 以及前足的X光片。
Among available FOPcase files, the common FOP ACVR1R206H mutation was documented in 41 subjects (22 M, 19 F; aged 0–48 years) with clinically diagnosed FOP and forefoot radiographs. Digit 1, Primary Ossification Centers | 趾1,初级骨化中心
在趾发育过程中,骨化中心会形成并产生趾的各个骨骼元素(跖骨和指骨)(Sarrafian,2011)。
发育出现的时间、骨化中心和指骨的最终数量是评估足趾骨骼发育的最常见方法。
人足的预期趾骨数量为 2-3-3-3-3,从趾 1 到 5,趾 1 的元素特别宽(图 1A、B、F)。
远端指骨的区别在于它们相对于内侧和近端指骨的矩形形状更像三角形。
每个趾骨由一个初级骨化中心 (POC) 组成,通过生长板近端连接到一个二级骨化中心 (SOC) (Sarrafian, 2011)。
第一指跖骨只有一个近端 SOC,而第 2-5 指的每个跖骨只有一个远端生长板和 SOC(Sarrafian,2011)。 SOC 通常以小的、圆形、正放射区域出现,随着时间的推移扩展成增厚的曲线,然后逐渐与其相关的骨骼元素融合。
During digit development, ossification centers form and give rise to the individual skeletal elements (metatarsals and phalanges) of the digits (Sarrafian, 2011). The timing of the emergence and the final number of ossification centers and phalanges are the most general means by which to assess skeletal development in the digits of the foot. The expected numbers of phalanges in human feet is 2-3-3-3-3, counting from digits 1 to 5, with the elements of digit 1 being particularly broad (Figures 1A,B,F). Distal phalanges are distinguished by their comparatively triangular shape relative to the rectangular shapes of medial and proximal phalanges. Each phalanx consists of a primary ossification center (POC) connected proximally to a single secondary ossification center (SOC) via a growth plate (Sarrafian, 2011). The first digit metatarsal has only a proximal SOC, whereas each metatarsal of digits 2–5 has only a distal growth plate and SOC (Sarrafian, 2011). SOCs typically emerge as small, circular, radio-positive regions that expand into thickened, curved lines over time before gradually fusing with their associated skeletal element. 在 41 名受试者中,我们所检查的趾 1 提供了比以往FOP中识别特征根据普遍性的改进图片。
这些特征(总结于表 1)包括几乎完全外翻的拇外翻(38/41;图 1C)、跖骨畸形(41/41;图 1C&#39;)、与近节指骨缺失相关的指间关节缺失(21/ 41;图 1C,E),以及第一跖骨头部中远端异位骨化中心 (EOC) 的存在(38/41;图 1E,3)。
Examination of digit 1 in our 41 subjects provided an improved picture of the prevalence of characteristics that were previously recognized in FOP. These features (summarized in Table 1) included nearly fully penetrant hallux valgus (38/41; Figure 1C), metatarsal malformation (41/41; Figure 1C’), loss of the interphalangeal joint associated with loss of the proximal phalanx (21/41; Figures 1C,E), and the presence of an ectopic ossification center (EOC) medio-distal to the head of the first metatarsal (38/41; Figures 1E, 3). 我们还确定了趾 1 的两种不同的常见病理:一种是指 1 的近节指骨缺失(单指拇趾;图 1C、C&#39;、G),另一种是存在指骨,但却畸形(双指拇趾;图 1D、D&#39;、H)。
尽管大多数脚的 X 光片显示出类似的双侧畸形,但 41 名接受检查的受试者中有一名在一只脚上有两个趾骨,但在另一只脚上却只有一个(图 1E,E&#39;)。
在余下的 40 名受试者中,单指骨20例,双指骨20例。
近节指骨缺失(单指骨)的受试者通常会表现出更为严重的拇外翻,而具有两个指骨(双指骨;p1 和 p2,分别为近节和远端指骨)的受试者拇外翻却不太严重。
在 15 岁及以上年龄时,所有病例在第一指(6/6;95% CI,61.0-100.0%)形成两个指骨(双指骨)的受试者会表现出两个指骨完全融合(图 1D&#39; 和补充图 1)。
并没有双指拇趾受试者会在 15 岁之前表现出这种融合(0/15;95% CI 0.0-20.4%)。
第一跖骨畸形表现为不对称或锯齿状的跖骨头和/或宽的骨干,缺乏从每一端到中轴的特征锥度(示例见补充图 1)。
We additionally identified two distinct general pathologies for digit 1: one in which the proximal phalanx of digit 1 is absent (monophalangeal hallux; Figures 1C,C’,G), and the other in which this phalanx is present but malformed (biphalangeal hallux; Figures 1D,D’,H). Although the majority of radiographs of the feet showed similar bilateral malformations, one subject of the 41 examined had both phalanges in one foot, but only one in the other (Figures 1E,E’). Of the remaining 40 subjects, 20 were monophalangeal and 20 were biphalangeal for the first digit. Subjects lacking the proximal phalanx (monophalangism) generally showed much more severe hallux valgus, whereas those with both phalanges (biphalangism; p1 and p2, proximal and distal phalanges, respectively) had less severe hallux valgus. At age 15 and older, all subjects who formed both phalanges (biphalangeal) in the first digits (6/6; 95% CI, 61.0–100.0%) showed complete fusion of the two phalanges (Figure 1D’ and Supplementary Figure 1). No subjects with biphalangeal hallux showed such fusion before age 15 (0/15; 95% CI 0.0–20.4%). Malformation of the first metatarsal presented as an asymmetric or jagged metatarsal head and/or a broad diaphysis lacking the characteristic taper from each end to the midshaft (examples shown in Supplementary Figure 1). FIGURE 1 | 图 1
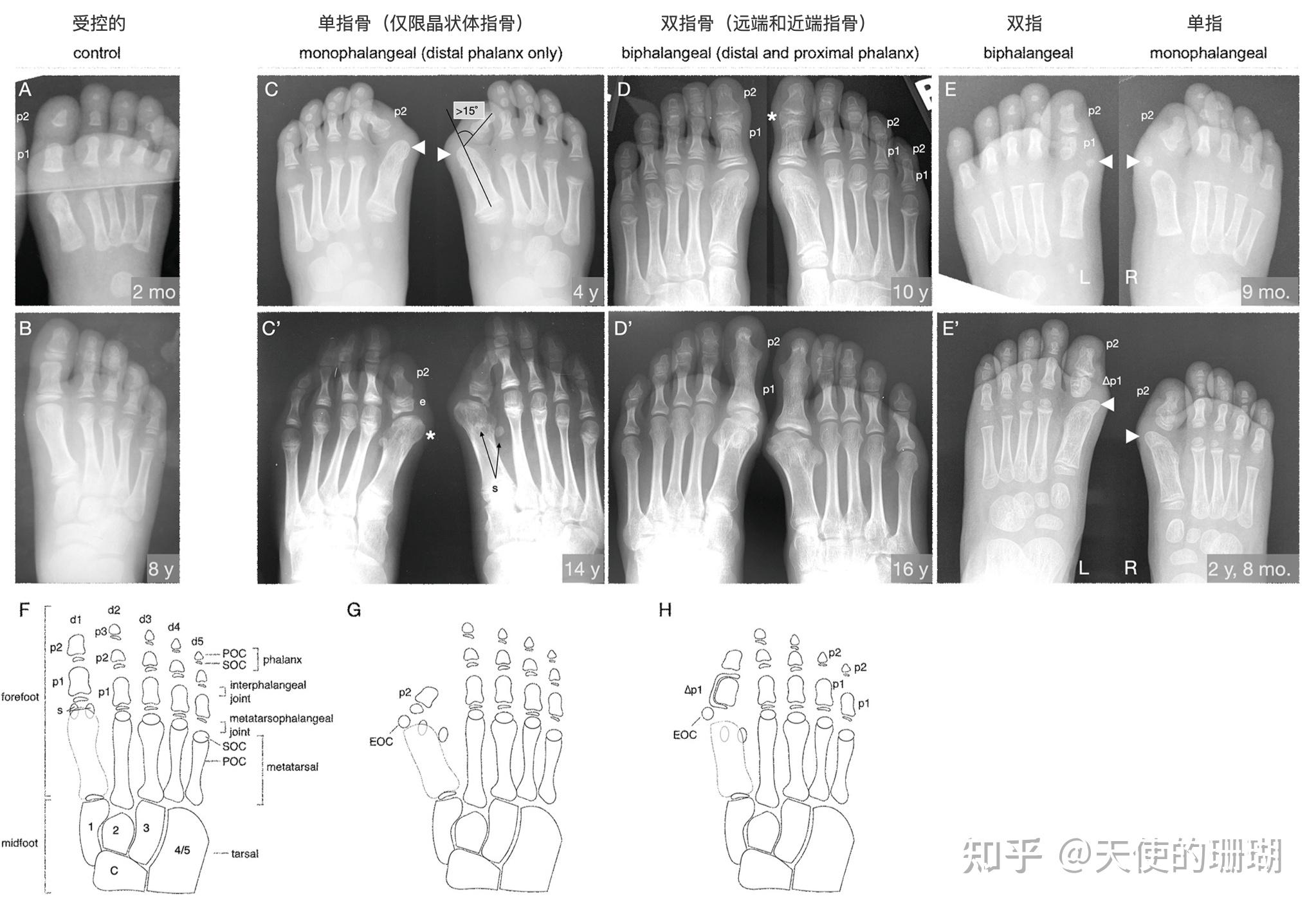
FOP伴随单指或双指拇趾的大脚趾畸形。
(A,B) 2 个月和 8 岁时的代表性受控射线照片。
注意除了第一个有两个之外,每个趾都存在三个指骨(p)。
(C-E)来自不同年龄的三个 FOP 受试者的 X 光片表现出了大脚趾畸形的两个主要表现:单指拇趾(仅 p2;C、E)和双趾拇趾(p1 和 p2;D、E)。
(C) 4 岁受试者的 X 光片显示双侧单指畸形,双足无 p1。严重的拇外翻很明显(拇外翻角度 > 15°,如图所示)。到了这个年龄,异位骨化中心(EOC;箭头)已经融合到了跖骨头上。
(C&#39;) 在 14 岁时,同一受试者表现出与剩余指骨相关的大骨骺 (e)、内侧偏斜的跖骨头部畸形(星号)和外侧偏斜的拇籽骨(s);腓骨籽骨清晰可见,而胫骨籽骨被跖骨掩盖。
(D) 受试者 10 岁时的 X 光片表现出双指畸形,第一指的两个指骨都存在于双脚中。
拇外翻是轻微的,与具有这种形态进展的其他受试者一致。
该受试者还出现了双指趾 4 和 5,虽然这不被认为是 FOP 的标志。
(D&#39;) 16 岁时,第一指的趾骨完全融合,这是 FOP 中双指拇趾的特征(详见补充图 1)。
(E) 一名受试者在 9 个月大时的成像,左脚有近端和远端指骨,右脚只有远端指骨。
注意近节指骨的不对称、无定形形状与 A 中矩形状的近节指骨、对称的形态形成了对比。
右脚显示比左脚更严重的拇外翻,但双脚在第一跖骨远端和内侧都有 EOC(箭头)。
(E&#39;) 两年后,EOC 都融合到跖骨头上。
(F-H)人类的足和前足骨骼元素的图示,(F)成年期的所有常见元素(对照),(G)单指 FOP 表型,和(H)双指 FOP 表型。
趾(d)从内侧到外侧编号为 d1 到 d5,指骨(p)从近端到远端编号。
通过 X 射线,可以看到每个元素的初级骨化中心 (POC),然后才能看到它们各自的次级骨化中心 (SOC)。
包括跗骨在内的中足元素仅供参考,并根据其各自的关节趾进行编号。
籽骨通常仅与拇趾相关,但可能出现在第二和/或第五指的跖趾关节处。
在 FOP 患者中看到的拇趾跖骨内侧和远端的特征性 EOC 标记在(G,H)中。
在 (E&#39;,H) 中,受 LEPB 或“delta phalanx”(也参见图 2)影响的指骨被标记为 1p1。
The FOP great toe malformation with monophalangeal or biphalangeal hallux. (A,B) Representative control radiographs at 2 months and 8 years of age. Note the presence of three phalanges (p) in each digit except the first, which has two. (C–E) Radiographs from three FOP subjects at different ages illustrate the two major presentations of the great toe malformation: monophalangeal hallux (p2 only; C,E) and biphalangeal hallux (p1 and p2; D,E). (C) Radiograph of a subject at 4 years of age shows bilateral monophalangism, with p1 being absent in both feet. Severe hallux valgus is evident (hallux valgus angle > 15 ◦ , illustrated). By this age, ectopic ossification centers (EOC; arrowheads) have fused to the metatarsal heads. (C’) At age 14, the same subject shows large epiphyses (e) associated with the remaining phalanx, medially deviated metatarsals with malformed heads (asterisk), and laterally deviated hallucal sesamoids (s); the fibular sesamoid is clearly visible, whereas the tibial sesamoid is masked by the metatarsal. (D) Radiographs of a subject at 10 years of age showing biphalangism, with both phalanges of the first digit present in both feet. Hallux valgus is minor, consistent with other subjects with this morphological progression. This subject additionally presents with biphalangeal digits 4 and 5, though this is not considered a hallmark of FOP. (D’) At age 16, the phalanges of the first digit have completely fused, which is characteristic of biphalangeal hallux in FOP (detailed in Supplementary Figure 1). (E) One subject, imaged at 9 months of age, presents with both a proximal and distal phalanx in the left foot and only the distal phalanx in the right foot. Note the asymmetric, amorphous shape of the proximal phalanx as contrasted with the rectangular, symmetrical morphology of the proximal phalanges in A. The right foot shows more severe hallux valgus than the left, but both feet have EOCs distal and medial to the first metatarsal (arrowheads). (E’) Two years later, the EOCs have both fused to the metatarsal head. (F–H) Illustrations of the skeletal elements of the human mid- and forefoot with (F) all usual elements in adulthood (control), (G) the monophalangeal FOP phenotype, and (H) the biphalangeal FOP phenotype. Digits (d) are numbered d1 to d5 from medial to lateral and phalanges (p) are numbered proximal to distal. By X-ray, primary ossification centers (POC) of each element are visible before their respective secondary ossification centers (SOC) can be seen. Midfoot elements, including the tarsals, are included for reference and are numbered according to their respective articulating digits. Sesamoids (s) are normally associated only with the hallux but may arise at the metatarsophalangeal joints of the second and/or fifth digits. The characteristic EOC medial and distal to the metatarsal of the hallux seen in FOP patients is marked in (G,H). In (E’,H), phalanges affected by LEPB or “delta phalanx” (also see Figure 2) are labeled as 1p1. Digit 1, Secondary Ossification Centers | 趾 1,二次骨化中心
指骨 SOC 在第 1 位平均出现在 10 个月到 2.3 岁之间,在第 2-5 位出现在 2.5 到 4.4 岁之间,男性晚于女性大约 6 到 12 个月。
SOC 最初表现为小的圆形正放射区域,随着时间的推移会扩展成增厚的曲线,然后逐渐与其相关的骨骼元素融合(Sarrafian,2011)。
在 FOP 的单指和双指病例中,第一指指骨的 SOC 在各种表现中经常出现畸形,包括近远轴的扩张(图 1C&#39;),具有不同程度不对称的沙漏状形状(图 1D),和增量排布(图 1E&#39;;也在下面和图 2 中详细说明)。
Phalangeal SOCs emerge on average between 10 months and 2.3 years of age in digit 1, and between 2.5 and 4.4 years of age in digits 2–5, with males lagging behind females by about 6 to 12 months. SOCs first appear as small, circular, radio-positive regions that expand into thickened, and curved lines over time before gradually fusing with their associated skeletal element (Sarrafian, 2011). In both monophalangeal and biphalangeal cases of FOP, SOCs of first digit phalanges were frequently dysmorphic in a variety of presentations, including expansion on the proximal-distal axis (Figure 1C’), an hourglasslike shape with varying degrees of asymmetry (Figure 1D), and delta phalanx (Figure 1E’; also detailed below and in Figure 2). 值得注意的是,16/21 (76%) 的两个第一指指骨的受试者也表现出一定程度的近节指骨的纵向骨骺支架 (LEPB)(图 2)。
LEPB 是一种罕见的骨骼畸形,其中一个骨骺沿骨干纵向延伸,并与对侧骨骺连续,通常导致相关解剖结构的中外侧偏差(Choo 和 Mubarak,2013 年)。
LEPB 在第一趾中出现极为罕见,仅报告了 9 例在 FOP 之外的病例(Neil 和 Conacher,1984;Low 等,2013;Verma 等,2014)。
在 21 名 FOP 受试者中的 3 名(14%)中,我们还发现了一种新的畸形,其中复合 LEPB 产生同心、骨化的半圆(图 3B,B&#39;)。
Of note, 16/21 (76%) subjects who have both first digit phalanges also exhibited some degree of longitudinal epiphyseal bracket (LEPB) of the proximal phalanx (Figure 2). LEPB is a rare skeletal malformation in which one epiphysis of a bone extends longitudinally along the diaphysis and is continuous with the opposing epiphysis, often leading to mediolateral deviation of the associated anatomy (Choo and Mubarak, 2013). LEPB is extremely rare in the first digit, with only 9 cases reported outside of FOP (Neil and Conacher, 1984; Low et al., 2013; Verma et al., 2014). In 3 of the 21 FOP subjects (14%), we also identified a novel malformation in which a compound LEPB produces concentric, ossified hemi-circles (Figures 3B,B’). 如前所述(Harrison 等,2005),几乎所有受试者(39/41;95%)在跖骨头远端和内侧都有 EOC。
在所有七名有多个年龄的 X 线照片的受试者中,包括一个连续五张 X 线照片的受试者(图 3),EOC 扩大并最终与第一跖骨头融合。
无论趾 1 的近节指骨是否存在(图 1),这种融合都会发生,这表明 EOC 不是错位或残留的指骨。
Nearly all subjects (39/41; 95%) had an EOC distal and medial to the metatarsal head, as previously described (Harrison et al., 2005). In all seven subjects for whom radiographs at multiple ages were available, including one with a series of five radiographs (Figure 3), the EOC expanded and ultimately fused with the head of the first metatarsal. This fusion occurred regardless of the presence or absence of the proximal phalanx of digit 1 (Figure 1), suggesting the EOC is not a misaligned or vestigial phalanx. FIGURE 3 | Progression of the FOP great toe malformation. | 图3 FOP大脚趾畸形的进展。
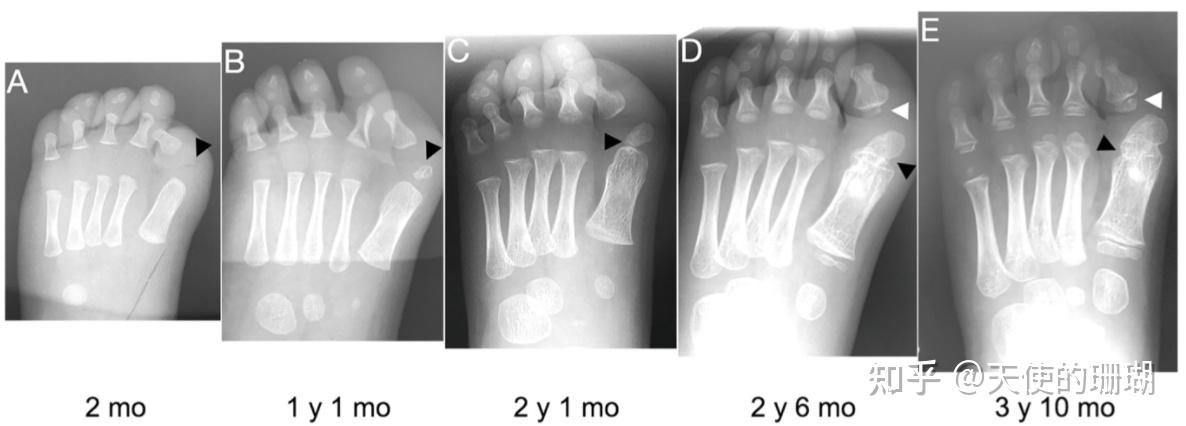
从出生到大约 4 岁的拇趾单指 FOP 受试者的 X 光片显示了拇外翻的持续性和异位骨化中心(EOC;黑色箭头)的进展。
(A) 出生时,EOC 明显是第一跖骨头远端和内侧的微小正放射区域。
(B,C)随着时间的推移,EOC 的大小和接近跖骨的程度增加,相对于指骨远端几乎没有生长。
(D) 剩余指骨的次级骨化中心(白色箭头 D、E)紧邻指骨形成,与 EOC 不同。
(E) 最后,骨骼似乎完全连接了 EOC 和跖骨(黑色箭头),将它们融合在一起。
FIGURE 3 | Progression of the FOP great toe malformation. Radiographs from a single FOP subject with monophalangeal hallux from birth to approximately 4 years of age illustrate the persistence of hallux valgus and the progression of the ectopic ossification center (EOC; black arrowheads). (A) At birth, the EOC is evident as a miniscule, radio-positive region distal and medial to the head of the first metatarsal. (B,C) Over time, the EOC increases in size and proximity to the metatarsal, with little to no growth distally relative to the phalanx. (D) The secondary ossification center of the remaining phalanx (white arrowheads D,E) forms immediately proximal to the phalanx, distinct from the EOC. (E) Finally, bone appears to fully bridge the EOC and the metatarsal (black arrowhead), fusing them together. Digits 2–5, Primary and Secondary Ossification Centers | 趾 2–5,初级和次级骨化中心
早前对 FOP 患者轴后指(第 2-5 指)的放射学研究发现,偶尔有远端指间融合和第五指内侧指骨缺失;然而,这种畸形在普通人群中并不少见(Ceynowa 等人,2018 年)。
为了评估 FOP 突变对脚的 2-5 指的影响,我们评估了指骨缺失、骨骺出现延迟和指间融合(表 2)。
与在一般人群中观察到这些特征相似,这些趾的指骨在 FOP 中从未出现过,除了趾 5 的中间指骨(22%)。
此外,远端指间融合发生的频率从内侧到外侧(趾 2-5)增加,骨骺延迟或缺失,从内侧到外侧的频率增加。
根据报告的研究,FOP 中这些趾变化的频率在普遍的范围内(Le Minor 等人,2016;Ceynowa 等人,2018)。
Previous radiographic studies of the post-axial digits (digits 2–5) of patients with FOP noted occasional distal interphalangeal fusion and absence of the fifth digit medial phalanx; however, such malformations are not uncommon in the general population (Ceynowa et al., 2018). To evaluate the effects of the FOP mutation on digits 2–5 of the feet, we assessed absence of phalanges, delayed appearance of epiphyses, and interphalangeal fusion (Table 2). Similar to observations of these features in the general population, phalanges of these digits were never absent in FOP except the middle phalanx of digit 5 (22%). Additionally, distal interphalangeal fusion occurred with increasing frequency from medial to lateral (digits 2–5) and epiphyses were either delayed or absent at increasing frequencies from medial to lateral. Based on reported studies, the frequencies of these digit variations in FOP are within the range of those within the general human population (Le Minor et al., 2016; Ceynowa et al., 2018). TABLE 1 Major abnormal features of the first digit in FOP patients.
表2. FOP患者第一指的主要异常特征。
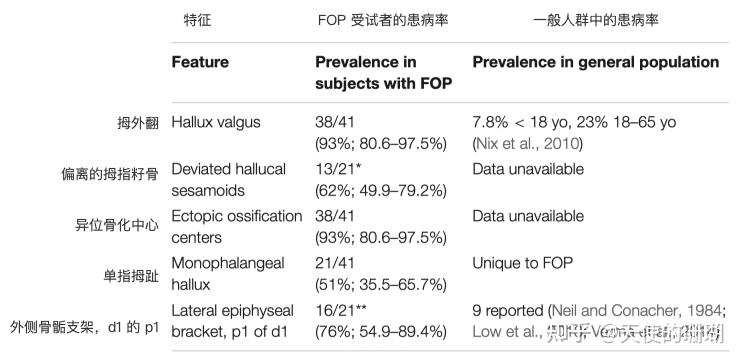
41 名分析对象的第一位数字中各种畸形的发生率。数据显示为总受试者的分数,然后是使用威尔逊/布朗检验计算的百分比和 95% 置信区间。
- 在研究中的 41 名患者中,只有 21 名具有完全可见的具备合理评估的拇籽骨。
- 41 名患者中只有 21 名有第一指的近节指骨,因此可以评估该特征。
Incidence of various malformations in first digits of 41 analyzed subjects. Data are presented as fraction of total subjects, followed by percent and 95% confidence interval calculated using the Wilson/Brown test.
Of the 41 patients in the study, only 21 had fully visible hallucal sesamoids that could be reasonably assessed.
*Only 21 of the 41 patients had a proximal phalanx of the first digit and therefore could be evaluated for this feature. TABLE 2 Frequency of anomalous radiographic features of the forefoot of individuals with FOP.
表2. FOP 患者前足异常影像学de频率特征。
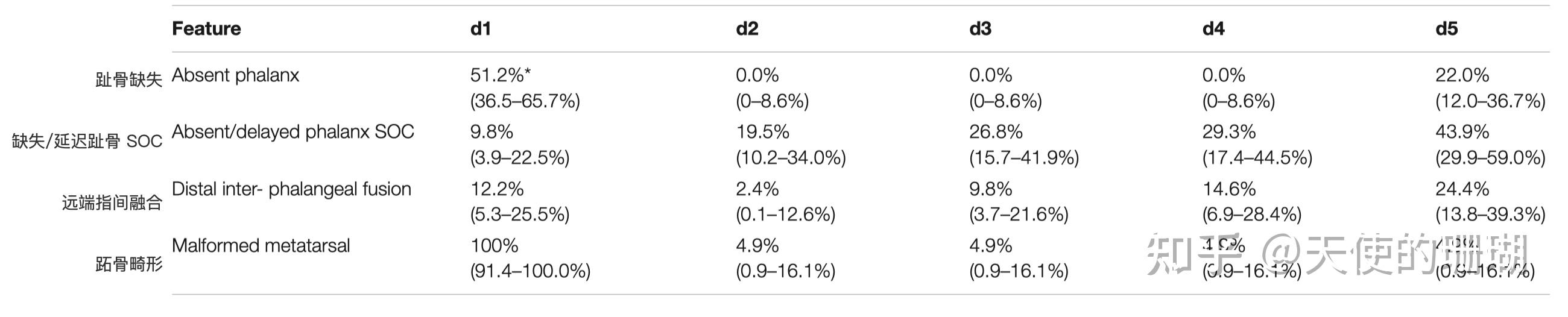
FIGURE 2 Longitudinal epiphyseal bracket in subjects with FOP. | 图 2 FOP 受试者的纵向骨骺支架。
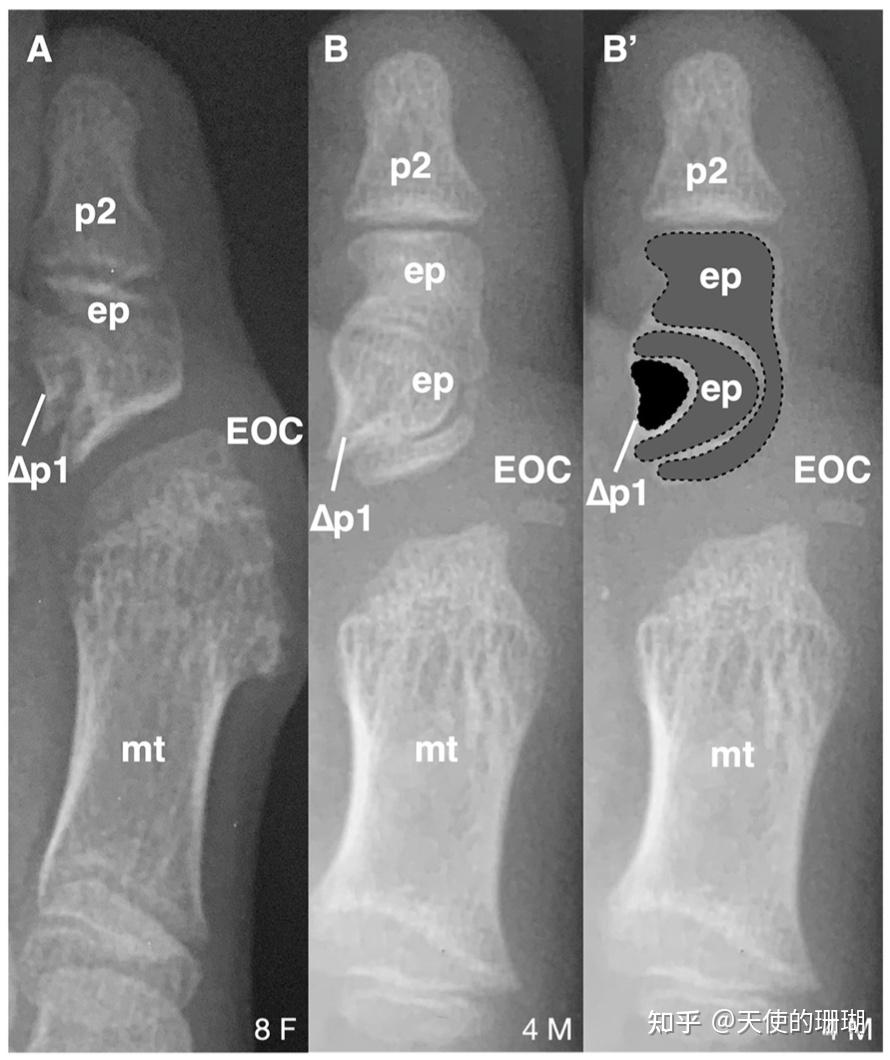
(A) X 光片显示 FOP 受试者大脚趾近节指骨 (p) 的纵向骨骺支架 (LEPB; ep)。
受 LEPB 影响的趾骨可称为三角趾骨,此处标记为 1p1。
跖骨头远端存在明显的异位骨化中心 (EOC)。
(B) 显示近节指骨的复合 LEPB 的 X 光片,在 (B&#39;) 中有清晰的轮廓。
虚线表示出现在同心半圆中的不同骨元素。
每个受试者的年龄(年)和性别(F,M),每个面板的右下角。
(A) Radiograph showing longitudinal epiphyseal bracket (LEPB; ep) of the proximal phalanx (p) of the great toe in a subject with FOP. A phalanx affected by LEPB may be referred to as delta phalanx, here labeled as 1p1. An apparent ectopic ossification center (EOC) distal to the metatarsal (mt) head is present. (B) Radiograph showing compound LEPB of the proximal phalanx, with outlines for clarity in (B’). Dotted lines denote distinct osseous elements occurring in concentric hemi-circles. Age (in years) and sex (F, M) of each subject, bottom right of each panel. 与第一指跖骨相比,FOP ACVR1 R206H 突变受试者的第 2-5 指跖骨畸形极为罕见。
然而,在具有 ACVR1 R206H 以外突变的罕见 FOP 病例中,骨性并指(融合)更为常见(Kaplan 等人,2009;Gucev 等人,2019)。
所检查的 41 名 ACVR1 R206H 受试者中有两名病例表现出跖骨并指,一名与趾 3 和 4 融合(图 4A),另一个与趾 3 和 4 之间以及趾 4 和 5 之间的融合(图 4B)。
此外,后一个受试者表现出明显的第五跖趾关节的关节外融合(图 4B)。
尽管跖骨通常有远端但没有近端次生骨化中心,但有两名 FOP 受试者在第 2-5 位的所有跖骨近端次生骨化中心呈现明显的近端次生骨化中心(图 4C)。
In contrast to metatarsals of the first digit, metatarsal malformations in digits 2–5 of subjects with the FOP ACVR1 R206H mutation were extremely rare; however, osseous syndactyly (fusion) is more common in rare cases of FOP with a mutation other than ACVR1 R206H (Kaplan et al., 2009; Gucev et al., 2019). Two of the 41 ACVR1 R206H subjects examined showed metatarsal syndactyly, one with fusion of digits 3 and 4 (Figure 4A), and the other with fusions between digits 3 and 4 as well as between digits 4 and 5 (Figure 4B). Additionally, the latter subject showed clear extra-articular fusion of the fifth metatarsophalangeal joint (Figure 4B). Although metatarsals normally have distal but not proximal secondary ossification centers, two FOP subjects presented with apparent proximal secondary ossification centers of all metatarsals in digits 2–5 (Figure 4C). DISCUSSION | 讨论
FOP 的大脚趾畸形自从最初与该疾病相关以来一直是一个谜(Rosenstirn,1918),但由于其相对于 FOP 中广泛的异位骨化的良性性质而很少受到关注。
在此,我们检查了具有 ACVR1 R206H 突变的 FOP 患者的指畸形的骨骼特征,以提供对该骨骼表型的更详细描述,从而更好地确定其病因,以及该突变对骨骼和关节上生物学其他方面的潜在影响。
此处介绍的发现确定了沿前足近端-远端轴的生长和形态改变模式,包括异常骨骼元素和异位骨化中心,与畸形、短大脚趾一致,这是 FOP 的特征性和诊断性的临床表现。
我们进一步确定,大脚趾畸形是由两种不同的表型引起的,单指和双指。
The great toe malformation of FOP has been an enigma since its first association with the disease (Rosenstirn, 1918) but has received little attention due to its benign nature relative to the extensive HO in FOP. Here, we examined the skeletal features of digit malformation in FOP patients with the ACVR1R206H mutation to provide a more detailed description of this skeletal phenotype and thus better determine its etiology and potential implications for the effects of the mutation on other aspects of skeletal and joint biology. The findings presented here identified altered patterns of growth and morphology along the proximal-distal axis of the forefoot including aberrant skeletal elements and ectopic ossification centers consistent with the malformed, short great toes that are a characteristic and diagnostic clinical feature of FOP. We further determined that the great toe malformations result from two distinct phenotypes, monophalangeal and biphalangeal. 尽管我们的横断面研究中的放射学证据不足以理解 FOP ACVR1 突变对骨骼和关节的全部后果,但小鼠模型中常见的 ACVR1-R206H 突变的表达会引起与在患者中观察到的类似的骨骼和关节畸形(Chakkalakal 等,2016)。
FOP 小鼠模型的趾 1 关节从出生开始就融合并发育放缓,这支持 ACVR1 对趾1 关节结构的适当规范很重要,并且 FOP 中 ACVR1 突变增加的 BMP 通路信号传导改变了骨骼元素。
Although the radiographic evidence in our cross-sectional study is insufficient to understand the full consequences of the FOP ACVR1 mutation on the skeleton and joints, expression of the common ACVR1-R206H mutation in mouse models induces similar bone and joint malformations in the digits to those observed in patients (Chakkalakal et al., 2016). FOP mouse models have digit 1 joints that are fused and diminished from birth, supporting that ACVR1 is important for the appropriate specification of joint structures in digit 1 and that increased BMP pathway signaling by the ACVR1 mutations in FOP alter the skeletal elements. ACVR1 在指定关节结构方面很重要的进一步证据源自于大多数患有 FOP 的人类受试者中存在的趾 1 中的异位骨化中心 (EOC)(表 1)。
如图 3 所示,该 EOC 似乎向跖骨头扩展,然后与跖骨头融合。
这种融合在视觉上与其他未受影响个体的正常生长板闭合一致;也就是说,从儿童期到青春期早期,EOC 和跖骨头之间的“接缝”很明显(图 1D-E;也图 3E),在青春期后期到成年期变得难以或无法检测到。
这一进展表明 EOC 是异位继发骨化中心 (SOC),通过异位生长板连接到跖骨头。
这种表型与 FOP 受试者内源性 SOC 的异常形态和生长一致。
在没有区分纤维软骨、肌腱和骺软骨的 MRI 补充数据的情况下,以及没有额外的射线照相观察平面的情况下,我们不能排除EOC 是一种异位籽骨,最终沿着其相关的肌腱组织融合到跖骨的这种可能性;
然而,我们的评估是,用数据更好地支持 EOC 通过生长板连接到跖骨头,因此构成了异位 SOC。
Further evidence that ACVR1 is important in specifying joint structures stems from the ectopic ossification center (EOC) in digit 1 that is present in the majority of human subjects with FOP (Table 1). As seen in Figure 3, this EOC appears to expand toward and then fuse with the metatarsal head. This fusion appears visually consistent with normal growth plate closure in other digits of unaffected individuals; that is, a “seam” between the EOC and metatarsal head is evident from childhood to early adolescence (Figures 1D–E; also Figure 3E) that becomes difficult or impossible to detect in late adolescence to adulthood. This progression suggests that the EOC is an ectopic secondary ossification center (SOC) that is connected to the metatarsal head via an ectopic growth plate. Such a phenotype is consistent with the aberrant morphology and growth of endogenous SOCs in subjects with FOP. In the absence of MRI data, which could help differentiate among fibrocartilage, tendon, and epiphyseal cartilage, as well as the absence of additional radiographic viewing planes, we cannot rule out the possibility that the EOC is an ectopic sesamoid that eventually fuses to the metatarsal along its associated tendinous tissue; however, our assessment is that the data better support that the EOC is connected to the metatarsal head by a growth plate, and thus constitutes an ectopic SOC. 如上所述,FOP 大脚趾畸形的一种潜在病因来自对籽骨的妥协,籽骨是支撑某些关节(尤其是膝关节和手指)的机械功能的小型骨化结构。
人类足部最常见的籽骨是胫骨和腓骨籽骨(统称为跖骨籽骨),它们与跖趾关节中第一跖骨头的腹沟相连。
少有籽骨也单独会出现在其他趾处(Bizarro,1921)。
我们关于趾 2 到 5 的数据无法最终表现 FOP 人群中的籽骨发育是否与一般人群中的不同;然而,FOP 受试者的拇籽骨经常横向偏离(可能是由于跖骨头畸形),这种情况会导致不平衡的机械外力导致拇外翻(Boike 等,2011)。
As mentioned above, one possible etiology for the malformed great toe in FOP comes from considering sesamoids, which are small, ossified structures that support the mechanical function of certain joints, particularly at the knees, and digits. The sesamoids found in human feet most frequently are the tibial and fibular sesamoids (collectively referred to as the hallucal sesamoids), which articulate with the ventral groove of the first metatarsal head in the metatarsophalangeal joint. Rarely, sesamoids also arise singly in other digits (Bizarro, 1921). Our data concerning digits 2 through 5 are unable to conclusively show whether sesamoid development in the FOP population deviates from that in the general population; however, hallucal sesamoids in FOP subjects were often laterally deviated (possibly as a result of the malformed metatarsal head), a condition that leads to unbalanced mechanical forces resulting in hallux valgus (Boike et al., 2011). 这项研究的一个早前未被认定的发现是大脚趾表型的两种不同表现,一种是单指的,一种是双指的。
起初,这似乎可以用个体受试者的背景遗传学来解释。然而,一名同时出现两种表现的受试者,一只脚,表现相反,FOP 突变及其导致的 BMP 通路信号增加,广泛的失调决定了第一指骨化的近端-远端模式的信号通路。
然后根据这些改变的参数随机确定骨化中心的数量和位置。
事实上,趾发育模式并不依赖于规定数量的骨骼元素,而是依赖于将 BMP 通路活性作为主导因素的复杂反应-阶梯扩散,其破坏会对趾和指骨数量和生长产生多种影响(Badugu 等人,2012;Raspopovic 等人,2014;Huang 等人,2016)。
One previously unrecognized finding from this study is the two distinct presentations of the great toe phenotype, one monophalangeal and one biphalangeal. This might at first seem likely to be explained by background genetics of individual subjects; however, one subject having both presentations, one in either foot, suggests that instead, the FOP mutation, and its resulting increased BMP pathway signaling, broadly dysregulates the signaling pathways that determine the proximal-distal pattern of ossification in the first digit. The number and positions of ossification centers is then determined stochastically from those altered parameters. Indeed, digit patterning is not dependent on a prescribed number of skeletal elements, but instead on complex reaction-diffusion gradients that incorporate BMP pathway activity as a major factor, the disruption of which can have a variety of outcomes on digit and phalanx number and growth (Badugu et al., 2012; Raspopovic et al., 2014; Huang et al., 2016). 我们在 FOP 患者的趾中注意到的每种表型——生长板位置和趾骨、籽骨趾骨和指骨数量——都是胚胎关节发育更为广泛和协调过程的组成部分(Grüneberg 和 Lee,1973;Ray 等人, 2015 年;Huang 等人,2016 年),并且与 FOP 人群中大量的关节发育不良、畸形和退行性关节病易感性的发现一致(Towler 等人,2019 年)。
尽管此处表述的表型之间的因果关系尚未最终确定,但这些数据为 FOP 患者大脚趾的发育表型提供了更全面和详细的视图,并为 ACVR1 和 BMP 通路信号传导在人类中骨骼和联合发育的作用提供了新的见解。
Each of the phenotypes that we have noted in FOP patient digits—growth plate placement and alignment, sesamoid alignment, and phalanx number—are components of the broader and coordinated processes of embryonic joint development (Grüneberg and Lee, 1973; Ray et al., 2015; Huang et al., 2016), and are consistent with findings of generalized joint dysplasia, malformation, and susceptibility to degenerative arthropathy in the FOP population (Towler et al., 2019). Although causal relationships among the phenotypes reported here cannot yet be conclusively established, these data provide a more comprehensive and detailed view of the developmental phenotype of the great toe in patients with FOP and provide new insight into the roles of ACVR1 and BMP pathway signaling in human skeletal and joint development. <hr/>多多爸( 微信: Aspirinic)
”天使的珊瑚FOP关爱之家“ 微信群主:
明明:微信号: gogoniluyo
方方:微信号: lengmou1314520
多多爸: 微信号: Aspirinic
微信群/公众号搜索:天使的珊瑚FOP关爱之家
注:为避免入错群,请家长/患者入群前,准备好ACVR1的基因检测报告。
<hr/>REFERENCES | 参考文献
Allen, R. S., Tajer, B., Shore, E. M., and Mullins, M. C. (2019). FOP-ACVR1 signals by multiple modalities in the developing zebrafish. Elife 9:e53761.
Badugu, A., Kraemer, C., Germann, P., Menshykau, D., and Iber, D. (2012). Digit patterning during limb development as a result of the BMP-receptor interaction. Sci. Rep. 2:991. doi: 10.1038/srep00991
Bizarro, A. H. (1921). On sesamoid and supernumerary bones of the limbs. J. Anat. 55(Pt 4), 256–268.
Boike, A., Schnirring-Judge, M., and McMillin, S. (2011). Sesamoid disorders of the first metatarsophalangeal joint. Clin. Podiatric Med. Surg. 28, 269–285. doi: 10.1016/j.cpm.2011.03.006
Ceynowa, M., Rocławski, M., Pankowski, R., and Mazurek, T. (2018). The prevalence and ossification pattern of the biphalangeal and triphalangeal lateral toes. Surg. Radiol. Anatomy 40, 1039–1045. doi: 10.1007/s00276-018-2027-z
Chakkalakal, S. A., Uchibe, K., Convente, M. R., Zhang, D., Economides, A. N., Kaplan, F. S., et al. (2016). Palovarotene inhibits heterotopic ossification and maintains limb mobility and growth in mice with the human ACVR1(R206H) Fibrodysplasia Ossificans Progressiva (FOP) mutation. J. Bone Miner. Res. 31, 1666–1675. doi: 10.1002/jbmr.2820
Choo, A. D., and Mubarak, S. J. (2013). Longitudinal epiphyseal bracket. J. Children’s Orthopaed. 7, 449–454. doi: 10.1007/s11832-013-0544-1
Cohen, R. B., Hahn, G. V., Tabas, J. A., Peeper, J., Levitz, C. L., Sando, A., et al. (1993). The natural history of heterotopic ossification in patients who have fibrodysplasia ossificans progressiva. a study of forty-four patients. J. Bone Joint Surg. Am. 75, 215–219. doi: 10.2106/00004623-199302000-00008
Grüneberg, H., and Lee, A. J. (1973). The anatomy and development of brachypodism in the mouse. J. Embryol. Exp. Morph. 30, 119–141.
Gucev, Z., Tasic, V., Plaseska-Karanfilska, D., Dimishkovska, M., Laban, N., Bozinovski, Z., et al. (2019). Severe digital malformations in a rare variant of fibrodysplasia ossificans progressiva. Am. J. Med. Genet. A 179, 1310–1314. doi: 10.1002/ajmg.a.61153
Harrison, R. J., Pitcher, J. D., Mizel, M. S., Temple, H. T., and Scully, S. P. (2005). The radiographic morphology of foot deformities in patients with fibrodysplasia ossificans progressiva. Foot Ankle Int. 26, 937–941. doi: 10.1177/ 107110070502601107
Huang, B.-L., Trofka, A., Furusawa, A., Norrie, J. L., Rabinowitz, A. H., Vokes, S. A., et al. (2016). An interdigit signalling centre instructs coordinate phalanxjoint formation governed by 5 ′ Hoxd–Gli3 antagonism. Nat. Commun. 7:12903. doi: 10.1038/ncomms12903
Kaplan, F. S., Xu, M., Glaser, D. L., Collins, F., Connor, M., Kitterman, J., et al. (2008). Early diagnosis of fibrodysplasia ossificans progressiva. Pediatrics 121, e1295–e1300. doi: 10.1542/peds.2007-1980
Kaplan, F. S., Xu, M., Seemann, P., Connor, J. M., Glaser, D. L., Carroll, L., et al. (2009). Classic and atypical fibrodysplasia ossificans progressiva (FOP) phenotypes are caused by mutations in the bone morphogenetic protein (BMP) type I receptor ACVR1. Hum. Mutat. 30, 379–390. doi: 10.1002/humu.20868
Le Minor, J.-M., Mousson, J.-F., de Mathelin, P., and Bierry, G. (2016). Non-metric variation of the middle phalanges of the human toes (II-V): long/short types and their evolutionary significance. J. Anatomy 228, 965–974. doi: 10.1111/joa. 12462
Low, K., Smith, J., Lee, S., and Newbury-Ecob, R. (2013). A mother and daughter with a novel phenotype of hand and foot abnormalities and severe pectus excavatum. Am. J. Med. Genet. A 161A, 2056–2059. doi: 10.1002/ajmg.a.36016
Mishima, K., Kitoh, H., Haga, N., Nakashima, Y., Kamizono, J., Katagiri, T., et al. (2014). Radiographic characteristics of the hand and cervical spine in fibrodysplasia ossificans progressiva. Intractable Rare Dis. Res. 3, 46–51. doi: 10.5582/irdr.2014.01009
Neil, M. J., and Conacher, C. (1984). Bilateral delta phalanx of the proximal phalanges of the great toes. a report on an affected family. J. Bone Joint Surg. Br. 66, 77–80. doi: 10.1302/0301-620x.66b1.6693482
Nix, S., Smith, M., and Vicenzino, B. (2010). Prevalence of hallux valgus in the general population: a systematic review and meta-analysis. J. Foot Ankle Res. 3:21. doi: 10.1186/1757-1146-3-21
Pignolo, R. J., Baujat, G., Brown, M. A., De Cunto, C., Di Rocco, M., Hsiao, E. C., et al. (2019). Natural history of fibrodysplasia ossificans progressiva: crosssectional analysis of annotated baseline phenotypes. Orphanet J. Rare Dis. 14:98. doi: 10.1186/s13023-019-1068-7
Raspopovic, J., Marcon, L., Russo, L., and Sharpe, J. (2014). Digit patterning is controlled by a Bmp-Sox9-Wnt turing network modulated by morphogen gradients. Science 345, 566–570. doi: 10.1126/science.1252960
Ray, A., Singh, P. N. P., Sohaskey, M. L., Harland, R. M., and Bandyopadhyay, A. (2015). Precise spatial restriction of BMP signaling is essential for articular cartilage differentiation. Development 142, 1169–1179. doi: 10.1242/dev. 110940
Rosenstirn, J. (1918). A contribution to the study of myositis ossificans progressiva. Ann. Surg. 68, 485–520.
Sarrafian, S. K. (2011). Sarrafian’s Anatomy of the Foot and Ankle: Descriptive, Topographic, Functional, 3rd Edn. Philadelphia, PA: LWW.
Schaffer, A. A., Kaplan, F. S., Tracy, M. R., O’Brien, M. L., Dormans, J. P., Shore, E. M., et al. (2005). Developmental anomalies of the cervical spine in patients with fibrodysplasia ossificans progressiva are distinctly different from those in patients with klippel-feil syndrome: clues from the BMP signaling pathway. Spine 30, 1379–1385. doi: 10.1097/01.brs.0000166619.22 832.2c
Schroeder, H. W., and Zasloff, M. (1980). The hand and foot malformations in fibrodysplasia ossificans progressiva. Johns Hopkins Med. J. 147, 73–78.
Shen, Q., Little, S. C., Xu, M., Haupt, J., Ast, C., Katagiri, T., et al. (2009). The fibrodysplasia ossificans progressiva R206H ACVR1 mutation activates BMP-independent chondrogenesis and zebrafish embryo ventralization. J. Clin. Invest. 119, 3462–3472. doi: 10.1172/JCI37412
Shore, E. M., and Kaplan, F. S. (2010). Inherited human diseases of heterotopic bone formation. Nat. Rev. Rheumatol. 6, 518–527. doi: 10.1038/nrrheum. 2010.122
Shore, E. M., Xu, M., Feldman, G. J., Fenstermacher, D. A., Cho, T. J., Choi, I. H., et al. (2006). A recurrent mutation in the BMP type I receptor ACVR1 causes inherited and sporadic fibrodysplasia ossificans progressiva. Nat. Genet. 38, 525–527. doi: 10.1038/ng1783
Towler, O. W., Shore, E. M., and Kaplan, F. S. (2019). Skeletal malformations and developmental arthropathy in individuals who have fibrodysplasia ossificans progressiva. Bone 23:115116. doi: 10.1016/j.bone.2019.115116
Verma, V., Batra, A., Singla, R., Gogna, P., Magu, N., and Gupta, R. (2014). Longitudinal bracketed epiphysis of proximal phalanx of the great toe with congenital hallux varus managed simultaneously with monorail external fixator: a case report. Foot Ankle Special. 7, 68–70. doi: 10.1177/1938640013502724 |
|